Osteoporosis
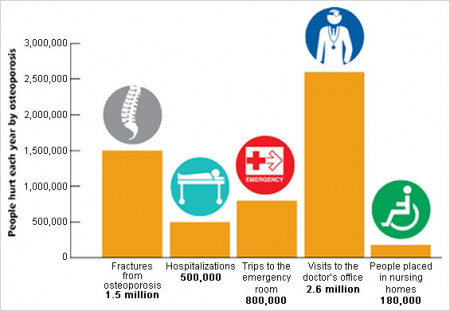
Osteoporosis is a disease in which the bones become weak and are more likely to break. People with osteoporosis most often break bones in the hip, spine and wrist. Senior patients commonly suffer from weakened (osteoporotic) bones, leaving them more frail and susceptible to fragility. The risk for osteoporosis increases with age, but there are no symptoms, and it frequently goes undiagnosed until you suffer a fracture.
Source: NIH's Osteoporosis and Related Bone Diseases National Resource Center
Risk Factors
Many risk factors can lead to bone loss and osteoporosis. Some of these things you cannot change and others you can. Risk factors you cannot change include:
- Gender. Women get osteoporosis more often than men.
- Age. The older you are, the greater your risk of osteoporosis.
- Body size. Small, thin women are at greater risk.
- Ethnicity. White and Asian women are at highest risk. Black and Hispanic women have a lower risk.
- Family history. Osteoporosis tends to run in families. If a family member has osteoporosis or breaks a bone, there is a greater chance that you will too.
There is some natural bone loss as women and men age. Bones can break or weaken if we don’t take action every day to keep them strong.
Risk factors you can change include:
- Sex hormones. Low estrogen levels due to menopause can cause osteoporosis in women. Low testosterone levels can bring on osteoporosis in men.
- Anorexia nervosa. This eating disorder can lead to osteoporosis.
- Calcium and vitamin D intake. A diet low in calcium and vitamin D makes you more prone to bone loss.
- Medication use. Some medicines increase the risk of osteoporosis.
- Activity level. Lack of exercise or long-term bed rest can cause weak bones.
- Smoking. Cigarettes are bad for bones, and the heart, and lungs, too.
- Drinking alcohol. Too much alcohol can cause bone loss and broken bones.
Prevention
To help keep your bones strong and slow down bone loss, you can:
- Be sure to get adequate calcium, Vitamin D and nutrients to support bone and muscle health.
- Exercise regularly to help maintain muscle strength and balance (check with your doctor first).
- Quit smoking and limit your alcohol intake.
Diagnosis
 A DEXA scan to measure bone mineral density is painless.
A DEXA scan to measure bone mineral density is painless.
A bone mineral density (BMD) test is the best way to determine your bone health. The most widely recognized BMD test is a dual-energy X-ray absorptiometry, or DEXA scan. It is painless—a bit like having an X-ray, but with much less exposure to radiation. It can measure bone density at your hip and spine. A DEXA scan can:
- Detect low bone density before a fracture occurs.
- Confirm a diagnosis of osteoporosis if you already have one or more fractures.
- Predict your chances of fracturing in the future.
- Determine your rate of bone loss, and monitor the effects of treatment if the test is conducted at intervals of a year or more.
Bone health and your quality of life
 Falling can be painful and upsetting, but if your bones aren't healthy, it can also be life-changing. If your bones aren't strong, falling may result in a hip fracture, which can impact your mobility, your independence and your quality of life. Statistics show that for up to a year after fracturing a hip:
Falling can be painful and upsetting, but if your bones aren't healthy, it can also be life-changing. If your bones aren't strong, falling may result in a hip fracture, which can impact your mobility, your independence and your quality of life. Statistics show that for up to a year after fracturing a hip:
- 90 percent of those who needed no assistance climbing stairs before the fracture will not be able to climb five stairs
- 66 percent won't be able to get on or off a toilet without help
- 50 percent won't be able to raise themselves from a chair
- 31 percent won't be able to get out of bed unassisted, and
- 20 percent won't be able to put on a pair of pants by themselves.
Unfortunately, only one in four adults who lived independently prior to the hip fracture will remain independent after the fracture is repaired.
Osteoporosis is not an inevitable part of life, even as you get older. Take action today to strengthen your bones. Work on eliminating your risk factors and developing diet and exercise habits that support bone health. Talk to your doctor about evaluating your bone density and steps you can take to improve it.
Cabell Huntington Hospital’s Senior Fracture Program was developed to provide rapid, thorough care and treatment to seniors who fracture a hip, with the goal of optimizing their recovery and ability to return to daily activities at their pre-fracture functioning level.
For more information about the program, please contact Becky Edwards at 304.399.1897 or Becky.Edwards@chhi.org.
